*This content has been reviewed by Professor Philip Calder (Faculty of Medicine, University of Southampton)
- Understanding Our Immune System. The immune system is the body’s defense system against infections and helps keep our bodies healthy.
- Nutrition and the Immune System. The immune system requires a varied, well-balanced diet in addition to sleep and physical activity to work properly. Including a variety of fruits and vegetables, whole grains, protein sources, and healthy fats can help support a healthy immune system.
- Sugars and the Immune System. The immune system uses glucose as a key source of energy. The media often claims sugars can suppress immune function but there’s not enough evidence to make this claim.
Understanding Our Immune System
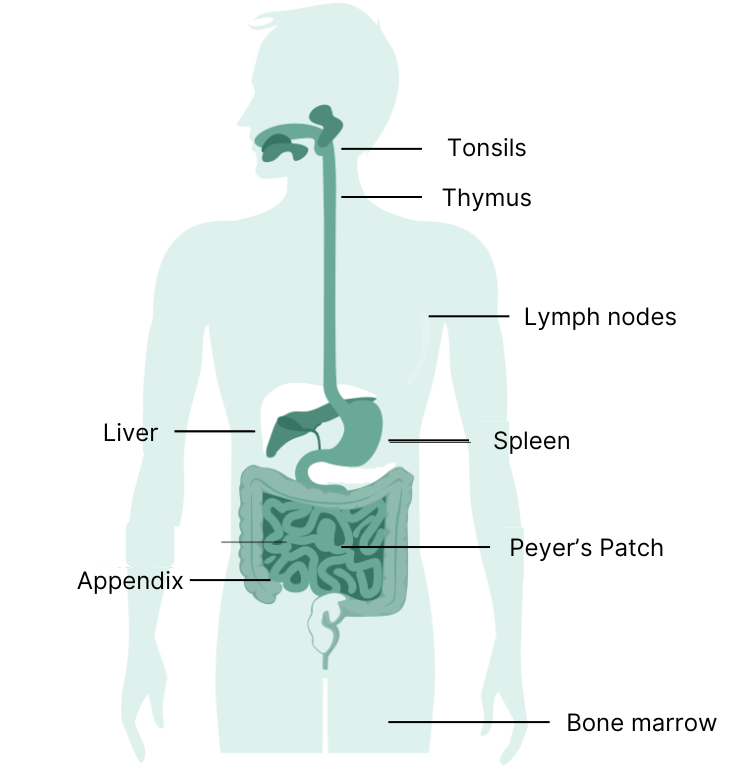 A well-functioning immune system is critical in helping our bodies to defend against infections or illness and assist with wound healing (1). The immune system consists of a complex network of cells and organs, which can be classified into the innate immune system and the adaptive immune system. These two parts of our immune system work as a team to fight infections and help keep our bodies healthy (1).
A well-functioning immune system is critical in helping our bodies to defend against infections or illness and assist with wound healing (1). The immune system consists of a complex network of cells and organs, which can be classified into the innate immune system and the adaptive immune system. These two parts of our immune system work as a team to fight infections and help keep our bodies healthy (1).
- The innate immune system is the physical, first-line of defense made up of skin, mucous membranes, stomach acid, and proteins in saliva, tears and urine as well as immune cells that can engulf bacteria or kill infected cells.
- The adaptive immune system is the second line of defense, composed of white blood cells that identify and fight off pathogens (e.g., harmful bacteria/viruses). Once these cells have been exposed to an antigen (e.g. part of a pathogen or vaccine that the immune system recognizes), they remember it and can fight these specific antigens off again more rapidly when encountering them in the future.
Several factors can impact the immune system. Some of them we can control, others we cannot (2). Examples include:
| Controllable Factors | Non-controllable Factors |
|---|---|
|
|
Inflammation is Part of the Immune System
Inflammation is an essential part of the immune system. There are two types of inflammation: acute and chronic.
- With acute inflammation, the body responds to injuries rapidly to fight off pathogens and promote tissue healing.
- In contrast, chronic inflammation occurs when inflammation is tuned up too high and lasts for a long time. Chronic inflammation may cause harm to healthy tissues and organs, and has been associated with obesity, heart disease, diabetes, cancer, arthritis, and bowel diseases (6-9).
Nutrition and the Immune System
While healthy eating looks different for everyone, incorporating a variety of foods into your daily diet will provide your body with the energy and nutrients it needs to
- Support the immune system, which is energy demanding
- Make new proteins (e.g. antibodies) and rebuild new cells
- Help immune cells to function well
Glucose is the primary source of energy for the immune system. When immune cells become more active, they use more glucose. There is a close link between glucose use and how well the immune system works.
In addition, key nutrients including many micronutrients (vitamins and minerals) have been shown to help either support immune function, or regulate inflammation, or both (2,5,6). These include:
- Fat-soluble vitamins: A, D, E, K, carotenoids;
- Water-soluble vitamins: B6, folate, B12, C;
- Minerals: zinc, iron, selenium, magnesium, and copper;
- Fatty acids: omega-3 fatty acids (e.g. EPA, DHA);
- Plant polyphenols.
Eating a range of whole grains, fruits, vegetables, protein sources, and healthy fats, such as found in the Mediterranean Diet, can help ensure you are getting enough energy and essential nutrients for optimal immune function (2, 7, 10, 11). The “Western Diet”, which is commonly high in energy density, fat, sugars, and red meat, and low in fruits, vegetables, and dietary fibre, has been associated with weaker immunity especially compared to a Mediterranean style diet (3).
Sugars and the Immune System
The immune system has a high energy demand and glucose is its preferred source of fuel (1). Starches and sugars are the main dietary sources of glucose. In healthy individuals, blood glucose levels are tightly controlled by many factors. However, either low or high levels of blood glucose can become harmful to the immune system (2). While there is often media attention suggesting a link between sugars consumption and impaired immune function, the evidence available is uncertain (12-15).
- Some studies suggested an association, but it is not clear that this is a cause-and-effect relationship, between a dietary pattern higher in sugars-sweetened beverages and markers of inflammation (12-14).
- A systematic review and meta-analysis, representing the highest level of scientific evidence, reviewed 13 intervention trials focusing on adults with and without Type 2 Diabetes or overweight and obesity to determine the effect of sugars (glucose, fructose, and sucrose) from foods or beverages on markers of inflammation (15). The findings showed no difference in the effect between different types of sugars. Notably, many studies used high amounts of sugars (e.g., 100 g of added sugars), which do not reflect normal eating patterns.
More research is needed to better understand the role of sugars as one component of an overall eating pattern on immune function.
For more information, additional resources include:
- Dietary Guidelines on Sugars
- Frequently Asked Questions About Sugar
- Sugars and Health: Overweight and Obesity
- Health Canada - Canada’s Food Guide
References
- Royall D, Smith MA. Immune System: Background. In: Aubrey V, Neuman D, Royall D, eds. Practice Evidence-Based Nutrition. 2019.
- Calder PC. Nutrition and immunity: lessons for COVID-19. Eur J Clin Nutr. 2021 Sep;75(9):1309-18.
- Myles IA. Fast food fever: reviewing the impacts of the Western diet on immunity. Nutr J. 2014Jun17;13(1).
- Christ A, Lauterbach M, Latz E. Western Diet and the Immune System: An Inflammatory Connection. Immunity. 2019;51(5):794–811.
- Calder PC, Carr A, Gombart A, Eggersdorfer M. Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect against Viral Infections. Nutrients. 2020;12(4):1181.
- Gombart A, Pierre A, Maggini S. A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection. Nutrients. 2020 Jan 16;12(1):236.
- Health Canada. Healthy eating recommendations [Internet]. Canada's Food Guide; 2020.
- Tsoupras A, Lordan R, Zabetakis I. Inflammation, not Cholesterol, Is a Cause of Chronic Disease. Nutrients. 2018;10(5):604.
- Pawelec G, Goldeck D, Derhovanessian E. Inflammation, ageing and chronic disease. Curr Opin Immunol. 2014 Aug;29:23-8.
- Royall D, Smith MA, Nelson V, Neuman D. Eating Habits for a Healthy Immune System [Internet]. PEN: The Global Resource for Nutrition Practice; 2021.
- Mayr HL, Tierney AC, Thomas CJ, Ruiz-Canela M, Radcliffe J, Itsiopoulos C. Mediterranean-type diets and inflammatory markers in patients with coronary heart disease: a systematic review and meta-analysis. Nutr Res. 2018 Feb;50:10-24.
- Schulze MB, Hoffmann K, Manson JE, Willett WC, Meigs JB, Weikert C, Heidemann C, Colditz GA, Hu FB. Dietary pattern, inflammation, and incidence of type 2 diabetes in women. Am J Clin Nutr. 2005;82:675–684.
- Hert KA, Fisk PS, Rhee YS, Brunt AR. Decreased consumption of sugar-sweetened beverages improved selected biomarkers of chronic disease risk among US adults: 1999 to 2010. Nutr Res. 2014;34:58–65.
- Kosova EC, Auinger P, Bremer AA. The Relationships between Sugar-Sweetened Beverage Intake and Cardiometabolic Markers in Young Children. J. Acad. Nutr. Diet. 2013;113:219–27. doi: 10.1016/j.jand.2012.10.020.
- Corte Della KW, Perrar I, Penczynski K, Schwingshackl L, Herder C, Buyken A. Effect of Dietary Sugar Intake on Biomarkers of Subclinical Inflammation: A Systematic Review and Meta-Analysis of Intervention Studies. Nutrients. 2018;10(5):606.


